Cervical cancer remains a significant burden in the healthcare community globally. According to the estimation by the World Health Organization, more than 600,000 new cervical cancer diagnoses are reported every year, and about 342,000 deaths annually. It is considered the fourth most prevalent cancerous disease among females (in 2022), and the majority is reported in low-and-middle-income regions.
Even though these figures are alarming, cervical cancer is one of the most preventable cancers if detected in time. cervical cancer detection and screening significantly help reduce mortality rates and improve outcomes for women everywhere.
What is Cervical Cancer? Symptoms and Causes
Cervical cancer originates from the cells of the cervix, which is the lower end of the uterus and part of the female reproductive system that leads to the vagina. This type of cancer is primarily due to persistent infection by certain strains of Human Papillomavirus (HPV). HPV infections are known to be self-limiting, but certain forms of the virus are believed to induce changes in the cervical cells that will eventually develop into cancer.
Generalized symptoms of cervical cancer include:
- Abnormal vaginal bleeding (after intercourse, between periods, or after menopause)
- Pelvic pain or discomfort during intercourse
- Unusual vaginal discharge
However, in the early stages, cervical cancer often does not present with symptoms, making cervical cancer detection through routine screening so critically important.
The Importance and Techniques of Cervical Cancer Detection
Regular screening is regarded as the best way by which early detection of cervical cancer can be established before any sign or symptom develops. An early cure and a higher survival rate are the products of early diagnosis and cure. There are two major ways in which cervical cancer is identified as follows: through HPV tests, although mainly in combination with the Pap test commonly done during a colposcopic examination.
1. HPV Tests
HPV tests detect the presence of high-risk types of HPV that are most likely to cause cervical cancer. Such a test might be done alone or together with a Pap test. HPV testing turns out to be very useful in identifying women who are at greater risk, even though they are apparently symptom-free.
2. Pap Test (Colposcopy)
Another important diagnostic tool for cervical cell changes that might lead to cancer is the Pap test, also referred to as the Pap smear. This test is conducted by gathering minute cell samples from the cervix, and then they are examined for any abnormalities. When such abnormalities are detected, the physician can move on to further evaluation through a colposcopic examination whereby the cervix can be closely looked for indications of disease under the magnifying glass of the digital colposcope.
Colposcopic Examination: When Is It Needed?
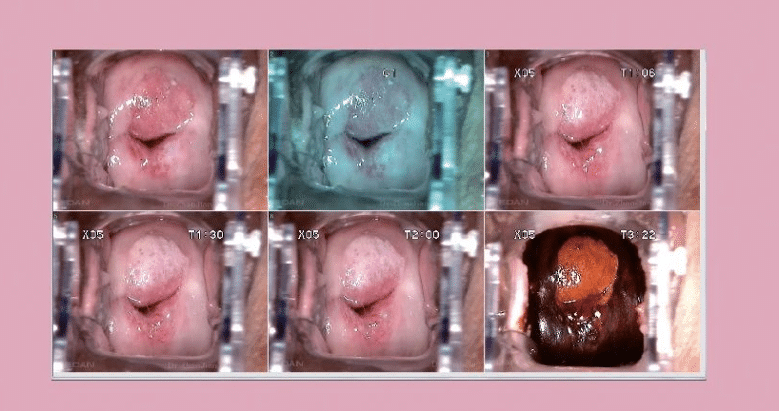
A colposcopic examination is a close look at the cervix. It is generally prescribed when abnormal cells are found on cervical screening tests or other symptoms that indicate a problem. This method utilizes a special gadget called a digital colposcope.
The digital colposcope is a clinical device first introduced by German physician Hans Hinselmann in 1925. Over decades, colposcopy has evolved into a gold-standard method for diagnosing lower genital tract diseases, including precancerous lesions and early-stage cervical cancer.
By magnifying images 10–60 times, a colposcope allows clinicians to observe minute abnormalities in the epithelial tissues of the cervix and reproductive organs, many of which are invisible to the naked eye. This painless and efficient procedure aids in precise diagnostics and significantly improves treatment outcomes, earning its place as an essential tool in women’s healthcare.
When to Screen?
The time of screening is an important factor in early detection. Guidelines vary with age:
- 21-29 years old: Pap test every 3 years. Routine HPV testing is not needed unless an abnormal finding exists from the Pap test.
- 30-65 years old: Co-testing with both the HPV and the Pap test every 5 years. Alternatively, she can have a Pap test alone every 3 years.
- Older than 65 years of age: Women older than 65 years who have had regular screening results that come out normal may no longer need screening. However, women with a history of cervical cancer should continue to be tested.
All women should undergo periodic screenings since cervical cancer detection prevents the transformation of abnormal cells into cancerous cells. Even those who have taken the vaccination against HPV have to continue with regular screenings because the vaccine does not protect all the types of HPV.
The EDAN C6A HD Digital Video Colposcope: Redefining Cervical Cancer Screening

For healthcare professionals committed to excellence in cervical cancer detection, the EDAN C6A HD Digital Video Colposcope offers a groundbreaking solution. Equipped with Sony’s advanced HD imaging technology, the C6A HD delivers unparalleled 1080P video resolution, enabling clinicians to discern intricate lesion details, vascular patterns, and real-time aceto-whitening reactions with utmost clarity. Let’s have a full picture of the gynecological examination helper.
✔ Exceptional Imaging Performance
C6A HD features A precision-engineered, high-definition lens that ensures lossless magnification, presenting every diagnostic detail with unmatched sharpness.
High-fidelity LED illumination replicates natural daylight, providing uniform lighting that minimizes glare and enhances the visibility of tissue structures.
✔ R-way Intelligent Evaluation System
EDAN’s proprietary R-way system introduces a quantifiable, standardized diagnostic process. This technology reduces dependency on clinician experience by offering objective evaluations based on advanced image analytics.
✔ Comprehensive Software Integration
The device features robust software tailored for clinical efficiency, supporting automated image capture, guided diagnostic workflows, and patient follow-up reminders.
Its reporting capabilities adhere to the 2011 IFCPC guidelines, providing pre-defined templates and customized options while generating PDF backups for medico-legal documentation.
✔ Ergonomic Design and Operational Efficiency
A gas-controlled articulating arm enables effortless positioning in tight clinical spaces, while a 360° observation range enhances examination flexibility.
The intuitive, foldable workstation design maximizes convenience for both clinicians and patients.
✔ Advanced Connectivity and Telemedicine Support
Fully compatible with DICOM 3.0 standards, the C6A integrates seamlessly with hospital PACS systems, enabling real-time data sharing for remote consultations and regional cervical cancer screening initiatives.
Conclusion
Regular screenings are the best prevention tool against cervical cancer; hence, women, especially those of specific ages, should follow the screening guidelines to catch any early problem. A healthcare provider can make a difference in saving lives when steps are taken proactively and modern technology such as digital colposcopes is used. Remember: regular screening is your best defence against cervical cancer – don’t wait to take charge of your health.